
★★★★★
We absolutely can’t thank you enough.
Powers & Santola was so knowledgeable and caring. I was so very fortunate to find such a great law firm.
Testicular cancer is the growth of cancer cells in one or both testicles (or testes). It usually occurs in young men. However, the disease can strike a man at any age.
Testicular cancer can be effectively addressed if detected at an early stage. The five-year survival rate for localized testicular cancer is 99.2 percent. At the regional stage, after it has spread to the lymph nodes, the survival rate is 96 percent. However, if testicular cancer has metastasized, or reached the distant stage, the survival rate falls to 73.1 percent.
If you suspect that a negligent delay in diagnosing testicular cancer has impacted you or a loved one, you deserve to have your case thoroughly investigated.
Contact Powers & Santola, LLP. We can provide a free and confidential review of your case and help you to understand your legal options.
What is
Testicular Cancer?
The testicles are made of several types of cells, each of which can develop into one or more types of cancer. However, more than 90 percent of testicular cancer cases develop in special cells known as germ cells. These are the cells that make sperm. Men have two main types of germ cell tumors (GCTs):
- Seminomas – These tumors grow and spread more slowly than non-seminomas. They are classified as classical (or typical) seminomas and spermatocytic seminomas. More than 95 percent of seminomas are classical. They usually occur in men between the ages of 25 and 45. Spermatocytic seminomas are rare and occur among men at an average age of 65. Spermatocytic tumors tend to grow more slowly. They are less likely to spread to other parts of the body than classical seminomas.
- Non-seminomas – These tumors usually occur in men between their late teens and early 30s. There are four main types of non-seminoma tumors, which are distinguished by how they look: Embryonal carcinoma, yolk sac carcinoma, choriocarcinoma and teratoma.
Most tumors are a mix of two or more different types (sometimes with a seminoma component as well).
Testicular cancer is rare, with about 8,800 new cases a year. It accounts for 0.5 percent of new cancers overall. With a five-year overall survival rate of 95.3 percent, it is also one of the more treatable forms of cancer.
How is
Testicular Cancer Diagnosed?
Just as women should regularly examine their breasts for lumps, men – particularly young men – should examine their testicles (in a warm shower) and talk to a doctor about any hard lumps or nodules (smooth rounded masses) or any change in the size, shape or consistency of their testicles. These could be signs of testicular cancer.
Otherwise, testicular cancer may cause:
- Feeling of heaviness in the scrotum
- A dull ache in the lower abdomen or groin
- Fluid in the scrotum that appears suddenly
- Pain or discomfort in a testicle or in the scrotum
- Lower back pain (in later stages of the cancer)
- Enlarged breasts (gynecomastia).
After examining a patient who reports symptoms that may be caused by testicular cancer, a doctor may order one or more of several diagnostic tests, including:
- Ultrasound – This test uses sound waves to produce images of internal organs. It is usually the first test done to check for testicular cancer. Based on the pattern of ultrasound echoes, a technician can distinguish between benign conditions (hydrocele or varicocele) and a solid tumor that could be cancerous.
- Blood test – Many testicular cancers make high levels of certain proteins such as alpha-fetoprotein (AFP) and human chorionic gonadotropin (HCG). These are known as “tumor markers.” When these tumor markers are in the blood, it suggests that there is a testicular tumor.
- Excisional biopsy – This test involves removal of testicular tissue to test for cancer cells. Surgery may also be performed to remove nearby lymph nodes to examine for spreading cancer cells.
- Imaging tests – If cancer is identified, further tests should be conducted to see whether the cancer has spread. This may be done with a CT, CAT, MRI or PET scan.
Why Does Missed or Delayed
Diagnosis of Testicular Cancer Occur?
Examining physicians or physician’s assistants are often under pressure to treat patients quickly. This may cause them to cut corners or rush through the more “routine” parts of an exam such as obtaining a patient’s medical history or symptoms. They may assume from one or two symptoms that they understand the problem and fail to order diagnostic tests that would reveal a testicular tumor.
Often, a missed or delayed diagnosis is caused by miscommunication. An order for diagnostic tests may be misplaced or misunderstood and delayed. A radiologist or technician may report test results incorrectly, or the physician may misread them. There are also cases of patients’ files, lab test results, MRI or CAT scans or biopsies being mislabeled. This can cause an incorrect diagnosis to be reported.
Another kind of missed diagnosis is an incorrect finding of cancer. Such a “false positive” may lead a patient to undergo treatment that is unnecessary, painful and potentially irreversible such as the removal of a testicle after the false diagnosis of testicular cancer.
What Are the Consequences
of a Missed or Delayed Diagnosis of Testicular Cancer?
If a misdiagnosis of testicular cancer occurs because the doctor mistakenly assumes the problem is only an infection, fails to consider the patient’s medical history while making a differential diagnosis or does not order the proper tests — or if the lab technician does not interpret the test results correctly — the patient’s situation and prognosis can grow significantly worse.
Treatment of testicular cancer may include surgery to remove the affected testicle, radiation therapy to kill cancer cells and shrink tumors or chemotherapy to kill cancer cells. It may include all three treatments. It is not hard to understand the potential psychological impact of testicular cancer on a young man.
Surgery to remove one testicle can cause emotional damage. Removal of both testicles could eliminate a single man’s opportunity to eventually reproduce. Chemotherapy may also leave a patient sterile or with low sperm counts.
Retroperitoneal lymph node dissection (RPLND) – the procedure to remove abdominal lymph nodes to diagnose the spread of testicular cancer – can cause a condition known as retrograde ejaculation. When this happens, semen will no longer come out of the penis during ejaculation.
It may be hard for such a “scarred” young man to attract a mate – either because of his emotional problems or the potential mate’s inability to deal with the effects of his cancer. (There are opportunities to store semen before treatment for testicular cancer and have children through artificial insemination. There are also implants available for men who have lost testicles to cancer.)
Get Help from a Delayed
Testicular Cancer Diagnosis Attorney
An attorney from Powers & Santola, LLP, can assist if you have been injured by a delayed, missed or false diagnosis of testicular cancer. Our New York law firm can help you to seek compensation for medical costs, pain and suffering and more if medical providers involved in your case were negligent or committed inexcusable errors.
Contact us today for a free and confidential initial consultation about your case and your legal options.
Sources / More Information
Other Practice Areas
Delayed Cancer
Diagnosis
Surgical
Malpractice
Wrongful
Death
Personal
Injury
Auto
Accidents
Medical
Malpractice
Changing Lives for the Better
When someone injures you, your life gets turned upside down. Suddenly, you may face a ton of medical bills. You may be unable to work or help out around the home. Others may need to care for you around the clock. Nothing is the same.
view all practice areas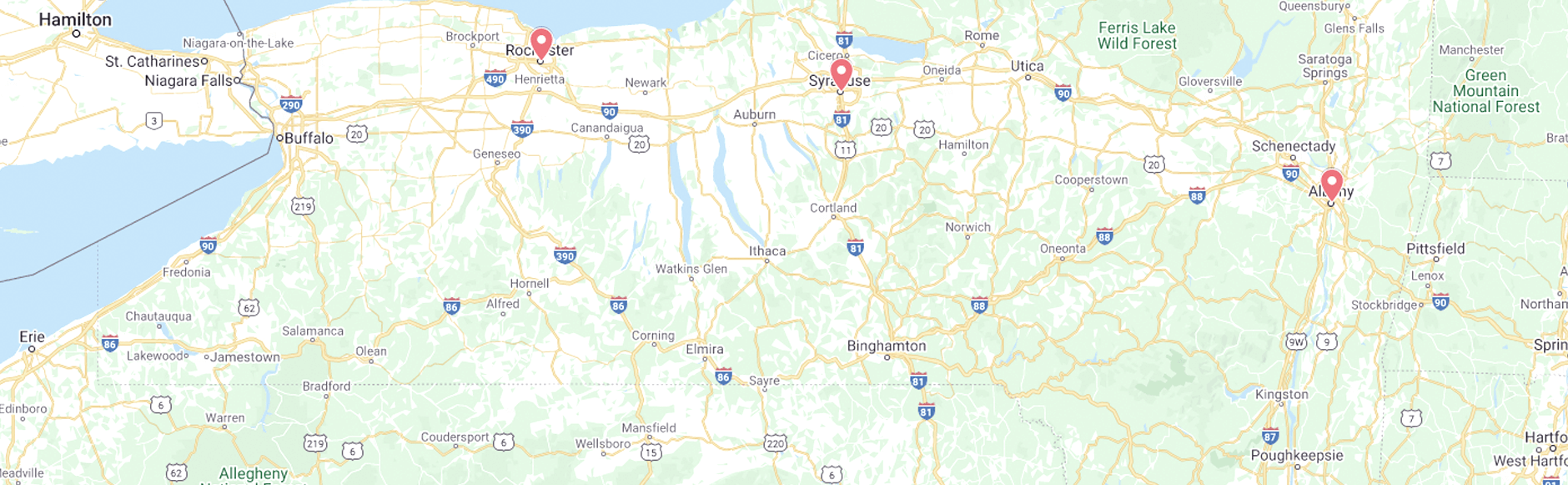
2024 Ⓒ Powers & Santola, LLP. All rights reserved. Privacy Policy | Site Map
The information you obtain at this site is not, nor is it intended to be, legal advice. You should consult an attorney for advice regarding your individual situation. We invite you to contact us and welcome your calls, letters and electronic mail. Contacting us does not create an attorney-client relationship. Please do not send any confidential information to us until such time as an attorney-client relationship has been established.