
★★★★★
We absolutely can’t thank you enough.
Powers & Santola was so knowledgeable and caring. I was so very fortunate to find such a great law firm.
Failure to Diagnose & Delayed Diagnosis Attorneys in Albany
Medical malpractice may occur when physicians and other medical professionals fail to diagnose cancer or from a delayed medical diagnosis. This diagnostic lapse can deprive a patient of needed medical treatments or surgery. Any delay in care can worsen the condition and lead to premature death. Contact our delayed medical diagnosis lawyers in Albany today.
For more than 30 years, Powers & Santola, LLP., has been helping patients and their families in Rochester, Albany, Syracuse and surrounding communities in upstate New York obtain justice for injuries caused by a failure to diagnose cancer or other serious medical conditions such as those listed below.
Other Commonly
Misdiagnosed Illnesses
Doctors are human. They make mistakes. But the stakes are pretty high when a physician diagnoses the wrong illness or misses a diagnosis altogether. Unfortunately, misdiagnoses happen at an alarming rate in New York and across the country.
Kaiser Health News reported last year on the prevalence of diagnostic mistakes. To say the least, the findings were troubling.
Somewhere between 10 to 20 percent of cases result in a misdiagnosis, Kaiser reported. In other words, a misdiagnosis occurs more often than a wrong site surgery or prescription drug error – two medical malpractice issues that often get more attention than misdiagnoses.
A misdiagnosis can be just as deadly as other medical errors. An estimated 28 percent of 583 diagnostic errors in one study were identified as life-threatening or resulting in death or disability. For every hour or day that passes without a correct diagnosis, the patient’s chances of increased illness or death grow.
Knowing the illnesses that doctors commonly misdiagnose could help you to take a more active role when dealing with your own doctor.
A recent study published in The Internet Journal of Family Practice sought to determine which misdiagnoses were most common. The researchers analyzed 62 studies to compare relative rates of misdiagnosis. Those rates were captured by malpractice cases and autopsy reports. The top 12 misdiagnosed illnesses were:
- Infections
- Myocardial infarctions (heart attacks)
- Cardiovascular disease
- Stroke
- Lupus
- Parkinson’s disease
- Lyme disease
- Depression.
- Sacroiliac joint dysfunction (a common cause of chronic hip and lower back pain)
- Celiac disease (a digestive and autoimmune disorder)
Many of these illnesses may come as a surprise. Cardiovascular disease, it would seem, should be easy to identify. But the symptoms of some illnesses can be vague. Sometimes, there are no symptoms at all.
With cancers, or neoplasms, the most commonly misdiagnosed types include breast cancer, melanoma, gynecological cancer, colorectal cancer and hematological cancer. An incredible 12 percent of cancer cases are initially misdiagnosed, according to a study published in 2005.
Addressing
the Problem
Fixing the harm done by a misdiagnosis is difficult. Also, many doctors are never made aware of their mistakes. Patients simply seek second and third opinions, changing providers when they are not satisfied with the diagnosis or result they are getting in one place. Without proper misdiagnosis tracking, we cannot know with any degree of certainty how big the problem is or why it is occurring.
This much is clear: Effective patient-doctor communication must take place in order to reduce the likelihood of a misdiagnosis. All symptoms must be communicated clearly by the patient, and doctors should be kept abreast of all related matters.
Regardless of whether a patient communicates symptoms to a physician, the duty to responsibly diagnose a condition rests with the doctor. When the signs of an illness are present and missed, or when a doctor negligently fails to follow up on symptoms, conduct proper testing and medical analysis – the results can be fatal.
Who Is Responsible
for My Delayed Diagnosis?
One challenge facing patients in medical malpractice cases is finding the doctor who is responsible for their care and injuries. With our medical system so streamlined and less personalized, it is common for a patient to see an admitting, attending and a referring physician during the course of treatment for one single injury.
If this is what occurred in your situation, seek out our legal assistance. We can look at all the factors involved in your care, including your medical records, to determine whether we can bring a claim against any or all of your doctors for the further harm they caused you. We will also utilize the knowledge of medical experts when making such determinations.
Contact Powers & Santola Albany Delayed Diagnosis Lawyers
Other Practice Areas
Delayed Cancer
Diagnosis
Surgical
Malpractice
Wrongful
Death
Personal
Injury
Auto
Accidents
Medical
Malpractice
Changing Lives for the Better
When someone injures you, your life gets turned upside down. Suddenly, you may face a ton of medical bills. You may be unable to work or help out around the home. Others may need to care for you around the clock. Nothing is the same.
view all practice areas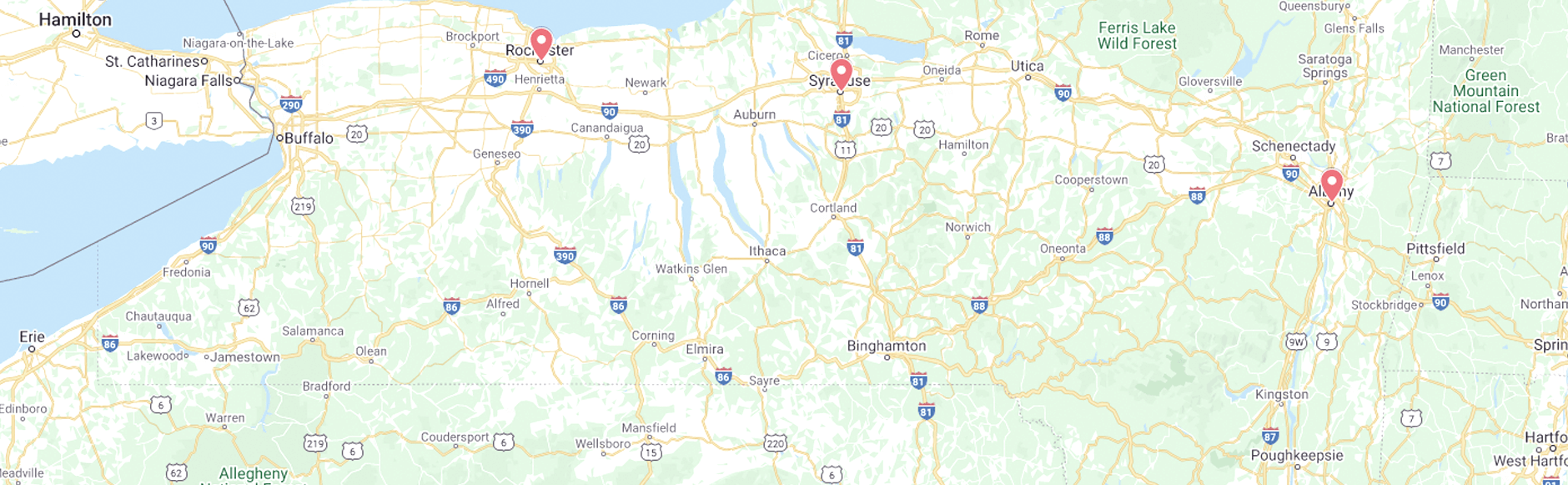
2024 Ⓒ Powers & Santola, LLP. All rights reserved. Privacy Policy | Site Map
The information you obtain at this site is not, nor is it intended to be, legal advice. You should consult an attorney for advice regarding your individual situation. We invite you to contact us and welcome your calls, letters and electronic mail. Contacting us does not create an attorney-client relationship. Please do not send any confidential information to us until such time as an attorney-client relationship has been established.