★★★★★
We absolutely can’t thank you enough.
Powers & Santola was so knowledgeable and caring. I was so very fortunate to find such a great law firm.
In times of medical emergencies, patients entrust their health and well-being to hospitals and the medical staff who work there. Unfortunately, hospital errors and mistakes are a fact of life. For patients, the consequences can mean serious injuries or illnesses, and in some cases lead to death. Contact our Albany hospital malpractice lawyer today.
Hospital negligence can lead to sepsis, staph infections, hospital-borne infections and blood clots, among other serious complications. Victims of hospital malpractice should remember that claims for hospital malpractice are subject to a statute of limitations. It is important to have any potential claim reviewed by a competent hospital malpractice attorney in Albany as soon as possible following an injury.
Injured by a Hospital Negligence Error?
Contact Powers & Santola Today
To schedule a free initial consultation with a New York hospital malpractice lawyer, contact Powers & Santola, LLP., online or call us today at 518-720-6188. We are here to listen and to help.
Other Practice Areas
Delayed Cancer
Diagnosis
Surgical
Malpractice
Wrongful
Death
Personal
Injury
Auto
Accidents
Medical
Malpractice
Changing Lives for the Better
When someone injures you, your life gets turned upside down. Suddenly, you may face a ton of medical bills. You may be unable to work or help out around the home. Others may need to care for you around the clock. Nothing is the same.
view all practice areas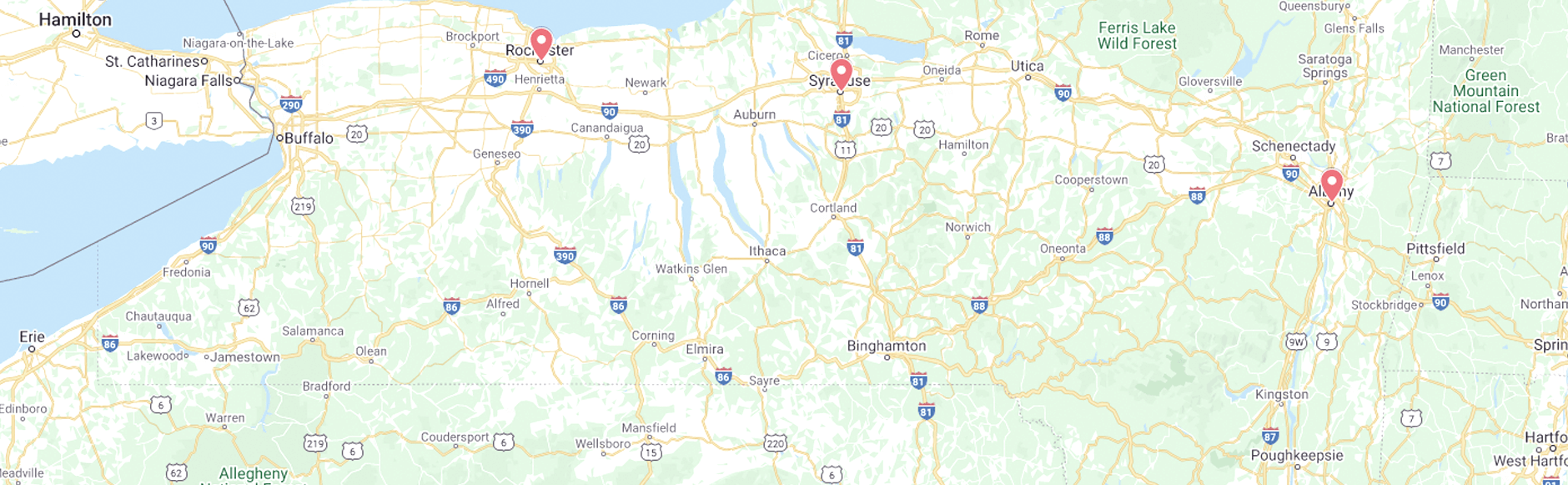
2024 Ⓒ Powers & Santola, LLP. All rights reserved. Privacy Policy | Site Map
The information you obtain at this site is not, nor is it intended to be, legal advice. You should consult an attorney for advice regarding your individual situation. We invite you to contact us and welcome your calls, letters and electronic mail. Contacting us does not create an attorney-client relationship. Please do not send any confidential information to us until such time as an attorney-client relationship has been established.