Most of us would agree: When serious medical errors occur, doctors should tell their patients. However, a survey published a few years ago revealed that many doctors do not share that view. In fact, many doctors actually think it is OK to tell patients something that is untrue.
In 2012, the journal, Health Affairs, reported a survey of nearly 1,900 practicing doctors from across the country. The researchers sought to gauge how widely doctors “endorse and follow” the Charter on Medical Professionalism’s requirement that doctors communicate with patients with “openness and honesty.”
As Health Affairs reported, most doctors in the survey said they believed that doctors should fully tell patients about the benefits and risks of medical interventions. However, a high number said they do not believe that doctors should be so forthcoming when treatment goes wrong.
Roughly 33 percent of the doctors said they did not “completely agree” that they should disclose “serious medical errors” to patients. Also, nearly 20 percent said they believed it may be all right to tell patients something untrue in some situations.
Medical Errors Occur Too Often
These survey results raise serious concerns – especially when one considers the high number of medical errors that occur in our country.
As The Washington Post reports, patient-safety researchers recently released a study which found that medical errors are now the third-leading cause of death in the United States.
Medical errors actually cause 251,000 deaths per year, claiming more lives than respiratory disease, accidents, Alzheimer’s disease, or stroke. Only cancer and heart disease cause more deaths than medical errors, according to the study, which was published in BMJ.
Back in 1999, the Institute of Medicine (IOM) issued a report that described preventable medical errors as an “epidemic” in our country. Interestingly, when that report came out, an estimated 98,000 medical error-related deaths occurred each year in the U.S. So, the number of medical error-related deaths in the U.S. has more than doubled today – the “epidemic” problem has only grown worse.
A lack of transparency may contribute to this growing problem. When mistakes are not disclosed, they cannot be adequately addressed by patients or the wider medical community.
Unfortunately, in a Washington Post article, Dr. Manoj Jain wrote that nearly everyone in the medical profession – colleagues, risk managers, and hospital lawyers – discourages doctors from admitting their mistakes. Also, medical schools fail to teach doctors how to disclose errors, according to Jain.
Why Should Doctors Tell Patients About Medical Errors?
Some of the most common medical mistakes today are missed diagnoses (such as a missed or delayed cancer diagnosis), medication errors, and surgical errors. Doctors and hospitals should tell patients and their families when these errors occur.
When medical professionals disclose errors, it gives patients the opportunity to get the medical treatment they need in order to address the error. It also creates a stronger, healthier bond between the doctor and the patient. This is especially true when the doctor not only acknowledges the error but also apologizes for it.
You Have Rights as a Patient in New York
When you are a patient, you should expect honesty from your doctor. The doctor should openly tell you about your condition and your treatment options. The doctor should also inform you about any mistakes or errors that occur in your diagnosis or treatment.
If you ask questions, and a doctor fails to provide you with honest answers, it exposes you to great harm. In other words: If you have no idea whether an error occurred, how can you address it?
What Can We Take Away from Michigan Doctor’s Medicare Fraud Case?
Dr. Farid Fata was a highly respected and, by all appearances, successful doctor in Michigan who specialized in oncology, or the treatment of cancer patients. According to a recent Newsweek article, Fata had built a practice that spanned seven cities and served more than 16,000 patients.
The problem: His medical empire, according to federal prosecutors, was largely built on lying to patients, including intentionally misdiagnosing patients with cancer so he could profit from administering chemotherapy drugs to them.
In September 2014, Fata pled guilty to health care fraud, money laundering and conspiracy to pay and receive kickbacks. In early July, he was sentenced in the U.S. District Court for the Eastern District of Michigan to a prison term of 45 years.
While the depths of Fata’s alleged misconduct are certainly extreme, his story reflects three significant problems that the medical community must address:
Too many potential conflicts of interest exist in modern medicine.
Newsweek reports that Fata allegedly prescribed more than “9,000 unnecessary injections and infusions to at least 553 patients over a six-year span” while his practice piled up “nearly $35 million in insurance billings,” including Medicare.
The Wall Street Journal states that roughly $25 million of those billings were directly attributable to Fata, making him the highest-paid oncologist in the country and the seventh-highest paid individual medical care provider overall.
Federal prosecutors claimed that Fata amassed his wealth by submitting insurance claims for services that were unnecessary, including prescribing chemotherapy to patients who did not have cancer but only needed observation, were already in remission or were terminally ill.
Unfortunately, as Newsweek points out, many doctors “bend their treatment decisions toward making the most money possible.” While this practice may not be fraudulent, as in Fata’s case, it raises concerns about conflicts of interest.
For example, a study reported in 2013 in the New England Journal of Medicine found that urologists who owned intensity-modulated radiation therapy (IMRT) services self-referred patients to this “expensive therapy” at a much higher rate than urologists who did not own IMRT services.
Patient health – not a doctor’s profits – should be the primary concern when a doctor makes a diagnosis and prescribes treatment. The potential for unethical or illegal conduct that harms patients exists where doctors can profit by making a particular diagnosis and treatment recommendation.
More transparency is needed in investigations of medical wrongdoing.
Another larger problem can be seen in the case of Dr. Fata: A lack of transparency in the investigation of medical negligence and other misconduct.
In Fata’s case, a nurse reported concerns about the doctor’s practices to the Michigan Bureau of Health Professions in 2010. A year later, she was told that an investigation found no wrongdoing by the doctor. Roughly two years passed before Fata was arrested by the FBI, Newsweek reports.
How do we know the case was thoroughly investigated by the agency? We don’t. According to Newsweek, the state will not release its investigative file for public inspection due to privacy laws that are meant to protect medical professionals.
As a result of such privacy laws, important information is kept from the public and exposes them to the risk of harm. For instance, how many patients would have gone to a different doctor or at least sought a second opinion if they had known about the 2010 allegations against Fata?
Would those in charge of regulating Michigan’s medical professionals be facing well-deserved scrutiny if it was revealed that the investigation of Fata was lacking?
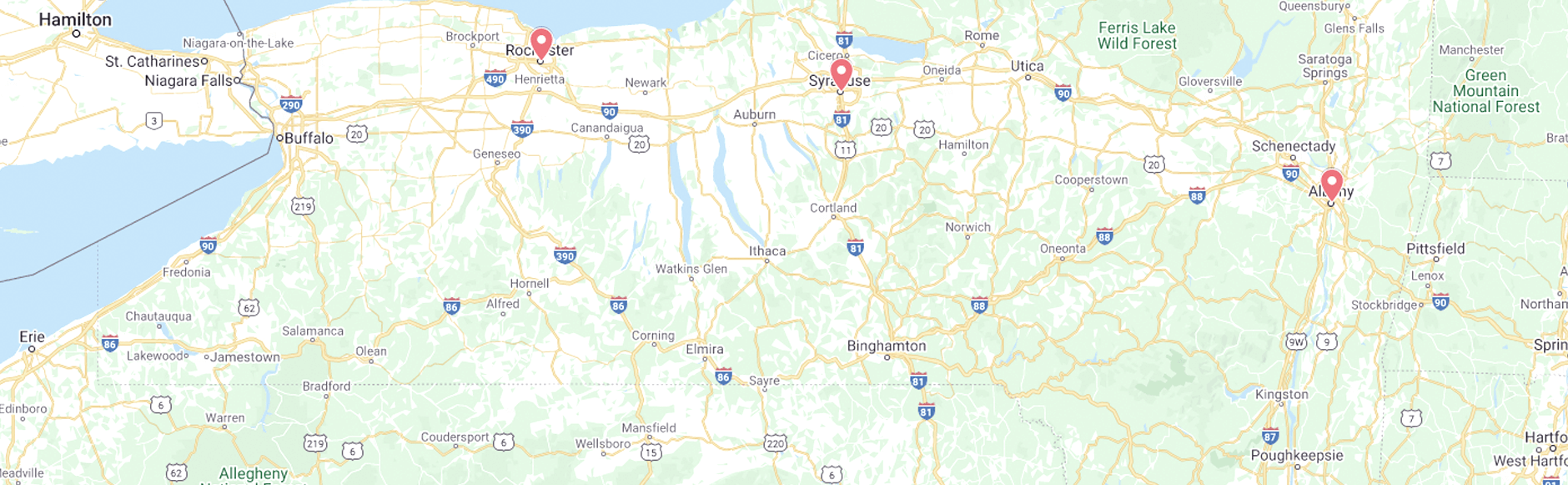
Here, in New York State, a 2014 report found that more needs to be done to inform patients about their doctor’s backgrounds. Currently, there is no requirement that New York patients be informed of disciplinary actions against the medical professionals they turn to for care.
Even though patients can find that information by going to the Office of Professional Medical Conduct’s website or calling its hotline, the report found it to be “highly unlikely” that patients in our state know about disciplinary actions on their doctor’s record.
Medical malpractice caps do not serve interests of justice.
Finally, it should be noted that Michigan, like many states in the U.S., places a cap on the non-economic damages that can be recovered in medical malpractice lawsuits.
Thus, despite enduring tremendous pain and suffering, patients harmed by Fata’s alleged misconduct will be fairly limited in the compensation they can potentially recover.
Fortunately, in New York State, there is no cap on medical malpractice damages. More states should follow suit. Justice is not served when victims are not fully and fairly compensated for the harm caused by negligent or reckless doctors.
Contact Us
If you would like to discuss suspected medical malpractice in a case that has harmed you or a loved one – specifically the delayed or missed diagnosis of cancer – please contact Powers & Santola, LLP. We would be glad to provide a free consultation about your case
When your doctor makes an error, you also have the right to pursue compensation for any losses that you have suffered as a result of that error. At Powers & Santola, LLP, our experienced New York medical malpractice attorneys are here to protect that right.
Call or reach us online today if you believe that a serious medical error harmed you or a loved one. We can provide a free consultation and immediately begin work on your case.